New Research Uncovers Groundbreaking Malaria Management Approach: Rendering Human Blood Lethal to Mosquitoes
In an unprecedented finding that might transform the global battle against malaria, researchers have discovered a novel technique to fight the disease—by making human blood a deadly agent for mosquitoes. The breakthrough centers around an already existing medication known as nitisinone, which, when present in a person’s bloodstream, can eliminate mosquitoes within hours of their bite.
This innovative strategy was revealed by scientists at the Liverpool School of Tropical Medicine, who studied the impacts of nitisinone on mosquitoes that consumed the blood of three individuals already utilizing the drug for a rare genetic condition. The results were remarkable: every mosquito perished within 12 hours of feeding, indicating that the drug effectively converted human blood into a mosquito-eradicating substance.
What Is Nitisinone?
Nitisinone is a medication currently approved for treating hereditary tyrosinemia type 1, a rare metabolic disorder. It functions by blocking the degradation of the amino acid tyrosine, resulting in a buildup of toxic substances within the body. Although its primary purpose is not related to infectious disease management, this newly identified side effect could have significant implications for public health.
How It Works Against Mosquitoes
When mosquitoes ingest blood containing nitisinone, the drug interferes with their ability to metabolize tyrosine, an essential process for their survival. Unlike traditional insecticides that target the nervous system, nitisinone influences metabolic processes, making it less likely to impact non-target insects such as bees and butterflies. This targeted action could position it as a more eco-friendly alternative compared to standard chemical sprays.
Advantages Over Existing Methods
The concept of leveraging medications to render human blood toxic to mosquitoes isn’t entirely novel. Ivermectin, another drug, has been assessed for similar applications. However, nitisinone presents several distinct benefits:
– Quicker Effect: Mosquitoes die within 12 hours of ingestion.
– Extended Longevity: The drug stays in the bloodstream for an extended duration, minimizing the need for frequent administration.
– Reduced Environmental Hazard: Since it does not target the nervous system, it poses a diminished risk to beneficial insects.
These characteristics position nitisinone as a compelling prospect for widespread drug administration in malaria-prone regions.
Potential for Large-Scale Impact
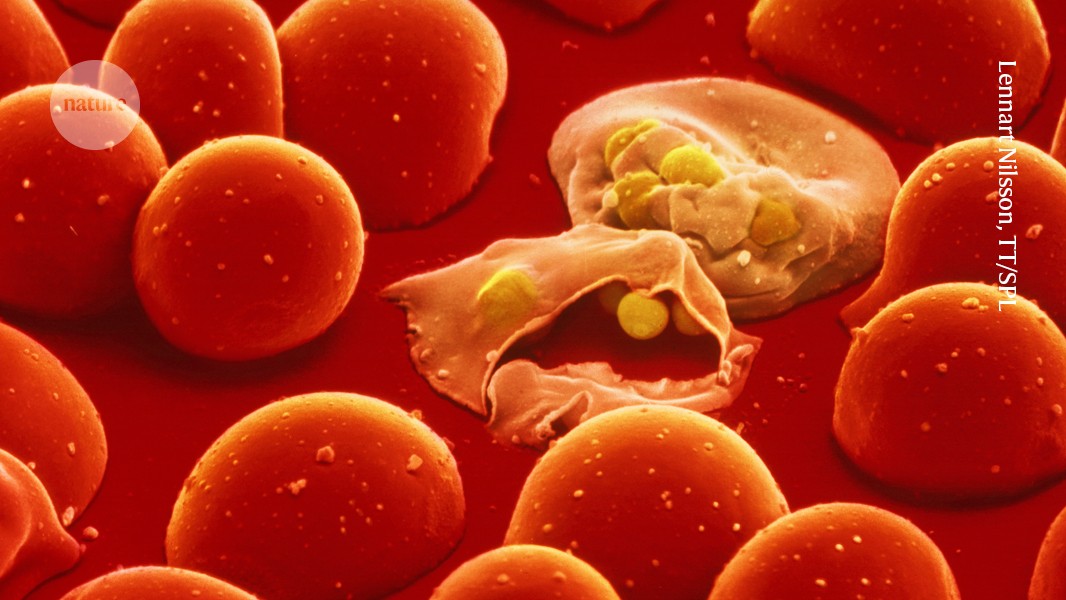
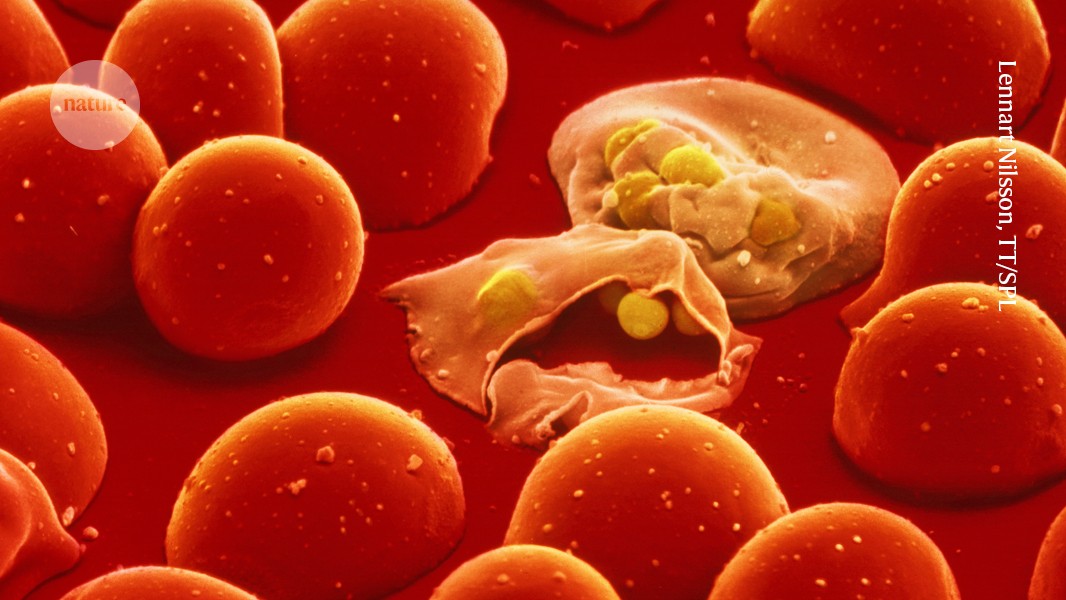
Malaria remains one of the deadliest diseases globally, especially in sub-Saharan Africa, where it takes hundreds of thousands of lives each year—many being children. Current control tactics include insecticide-treated bed nets, indoor spraying, and reducing mosquito breeding sites. While these strategies are effective, they encounter obstacles such as insecticide resistance and logistical challenges.
Transforming humans into mosquito eradicators reverses the typical approach. Rather than protecting individuals from bites, this strategy turns the act of biting into a death sentence for the mosquito. If applied on a large scale, it could drastically lessen mosquito populations and disrupt malaria’s transmission cycle.
Challenges and Considerations
Despite its promise, leveraging nitisinone as a tool for vector control is not without challenges:
– Ecological Considerations: Long-term impacts on ecosystems require comprehensive evaluation.
– Resistance Development: Mosquitoes may ultimately evolve to resist the drug, reducing its efficacy.
– Public Health Logistics: Coordinating mass drug distribution demands meticulous planning to prevent misuse and ensure fair access.
Moreover, researchers emphasize the necessity of ongoing surveillance and supplementary strategies to avoid over-dependence on a single method.
What’s Next?
Since nitisinone is already approved for human application, the pathway to broader testing and potential implementation is more straightforward than for a new drug. Future investigations will concentrate on determining optimal dosages, assessing long-term safety, and evaluating the drug’s effectiveness in practical scenarios.
If successful, nitisinone could be integrated into current malaria control initiatives, offering a robust new instrument in the global endeavor to eradicate the disease.
Conclusion
The revelation that a commonly used medication can convert human blood into a mosquito-destroying agent unveils a thrilling new avenue in the struggle against malaria. While hurdles persist, the possible advantages of this methodology—particularly in high-burden areas—are immense. By transforming the human host into a weapon against the mosquito vector, researchers may have pioneered a pivotal strategy in the fight against one of humanity’s oldest and most lethal adversaries.
As further studies progress, the world will be closely observing to see if this innovative approach can aid in achieving a malaria-free future.